TTP CLINICAL NURSING UPDATE AND REFRESHER / September 2018
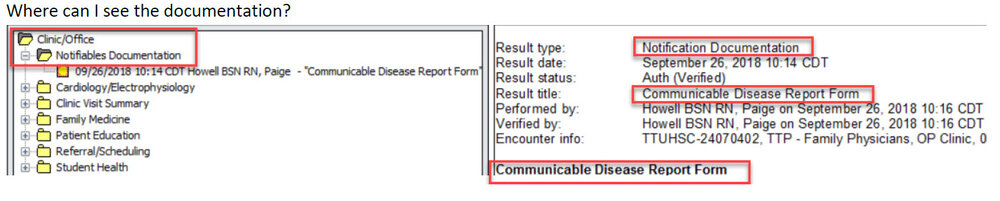
To report Patient Treatment of Notifiable Conditions to Lubbock Health Department, TTP Clinical Nursing Staff should follow these required guidelines to #1) document treatment and #2) complete notification process to the Lubbock Health Department:
Open patient chart on the correct clinical encounter.
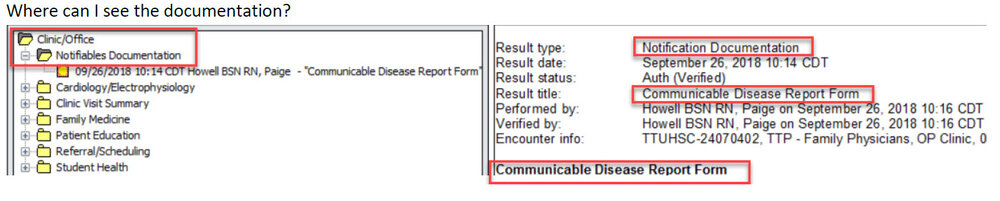
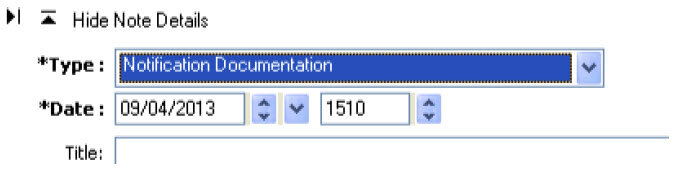
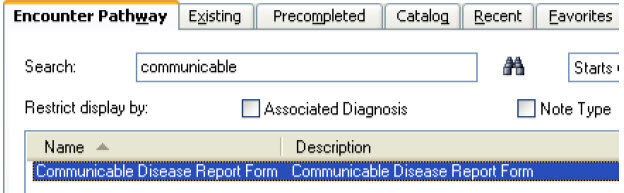
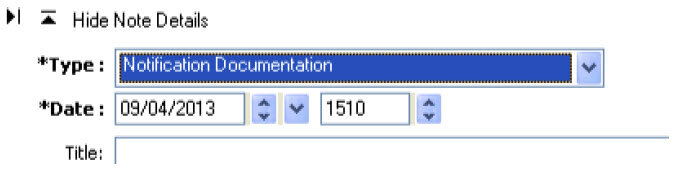
Add a new power note. Select Notification Documentation as the note type.
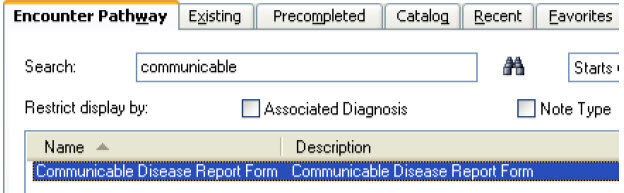
 Select the Communicable Disease Report Form Encounter pathway.
Select the Communicable Disease Report Form Encounter pathway.
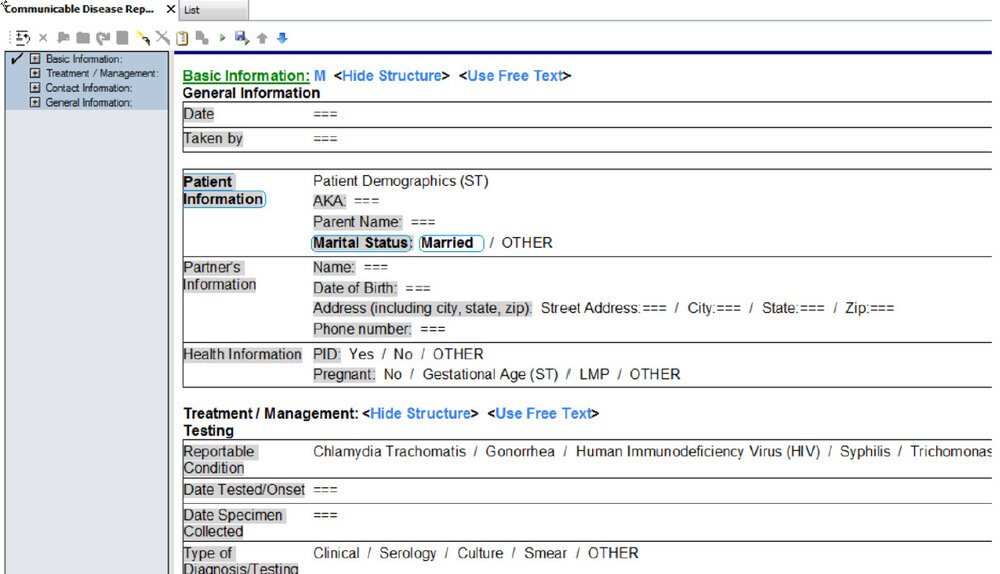
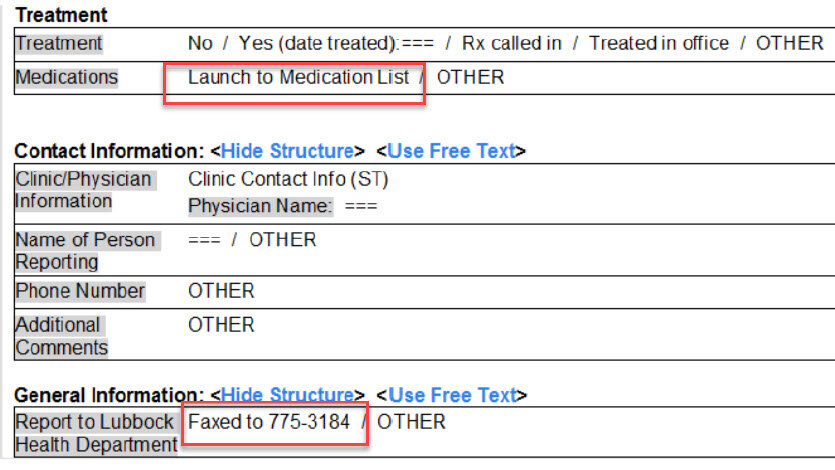
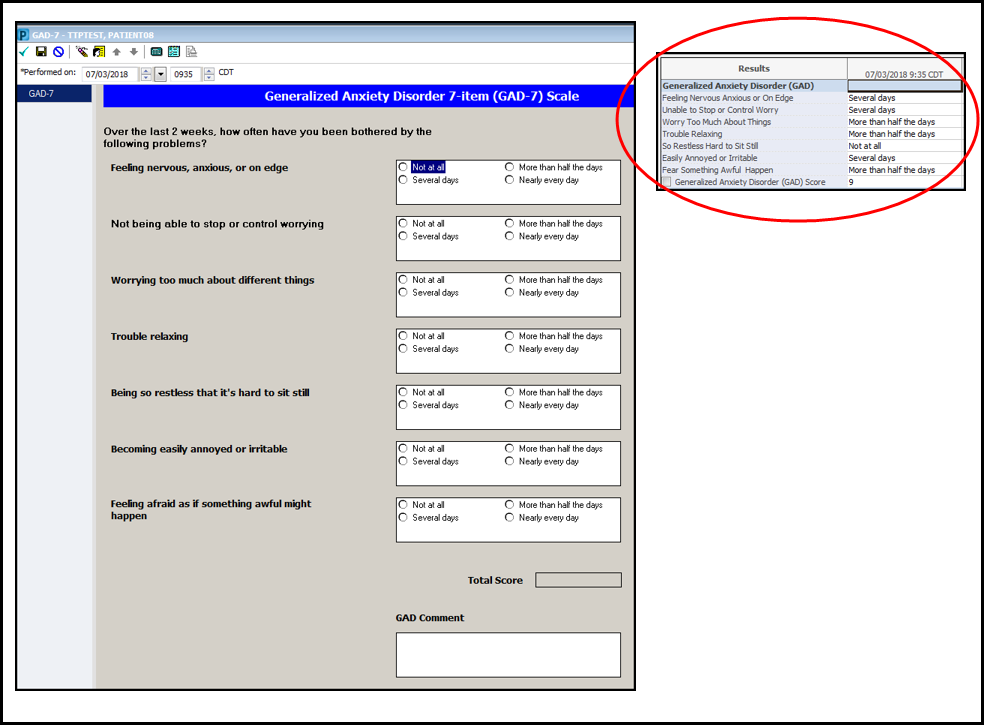
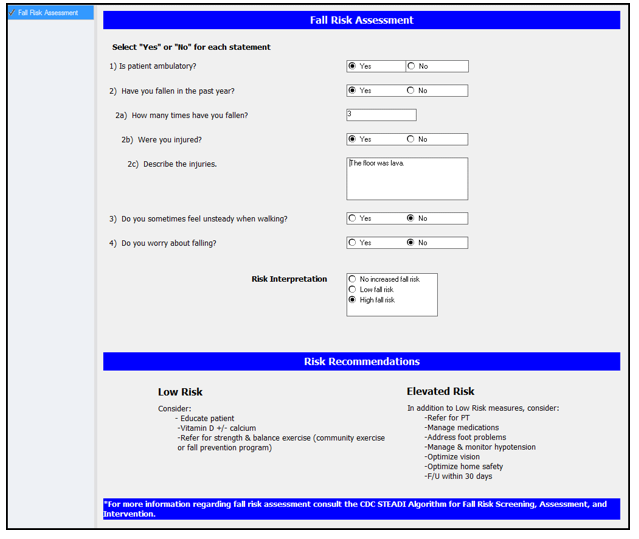
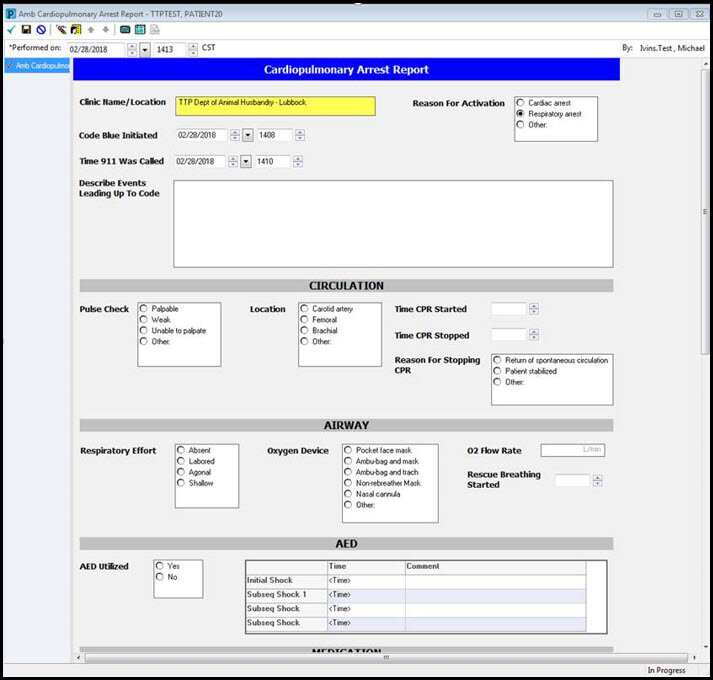
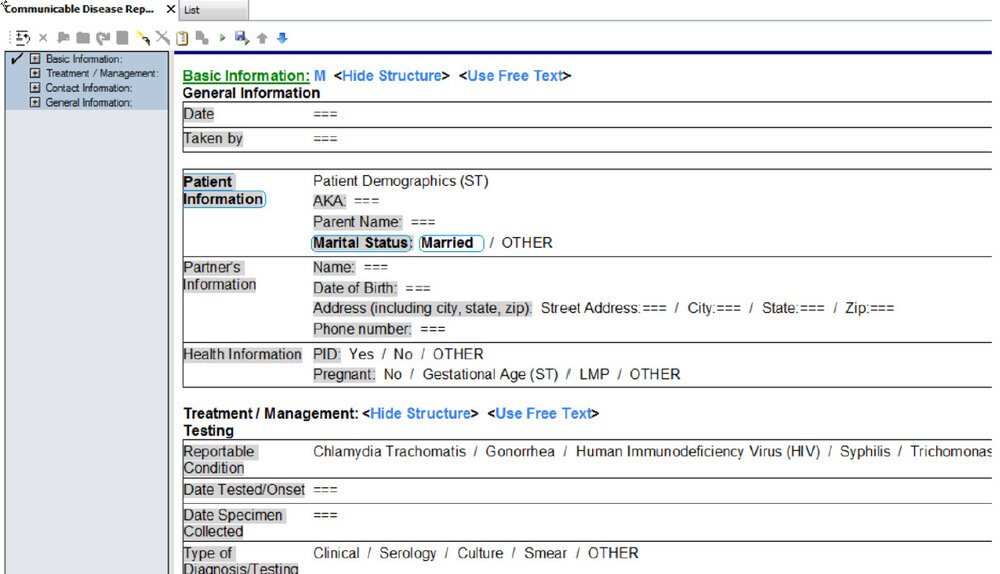
Fill out the custom note as required utilizing the smart templates (ST), bringing in all vital reportable information from the patient’s chart.
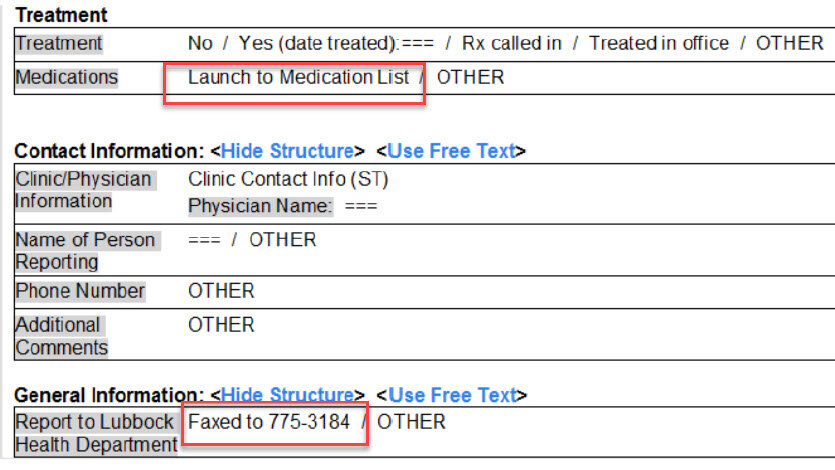
Option of: Faxed to Lubbock Health Department @ fax # 806 775 3184.**This is documentation purposes only ***
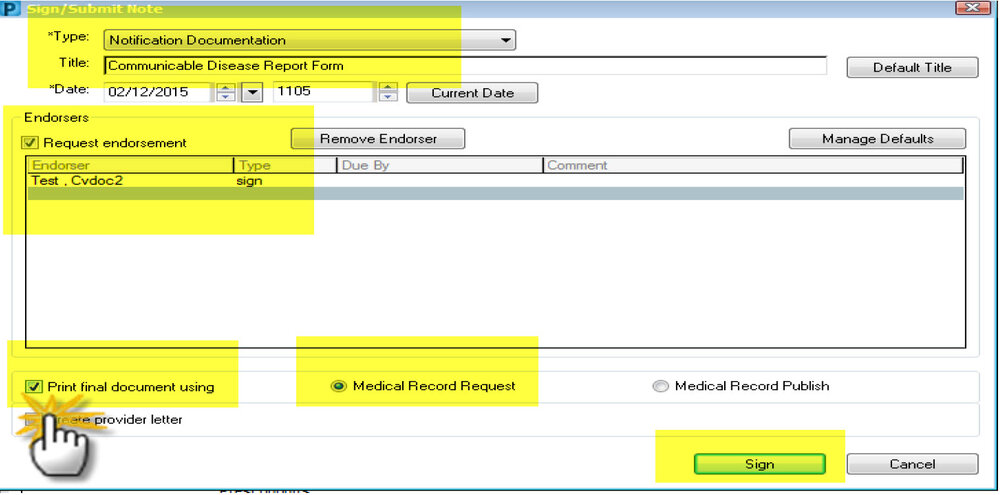
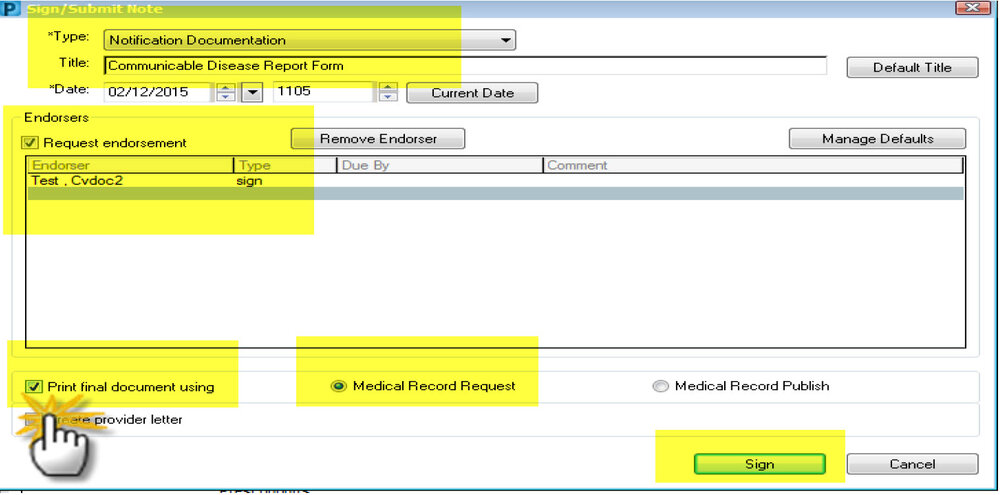
Sign the power note when finished, and request signature by provider as notification of reporting.
VERY VERY IMPORTANT: When signing your note, you MUST check the box at the bottom that states – PRINT FINAL DOCUMENT USING. THE MEDICAL RECORD REQUEST OPTION WILL AUTOMATICALLY DEFAULT. Now you may click SIGN and submit your note.
These steps are critical in telling the Cerner System how and where to fax your patient’s power note to the Lubbock Health Department.
One Time Set-up for Your Defaults:
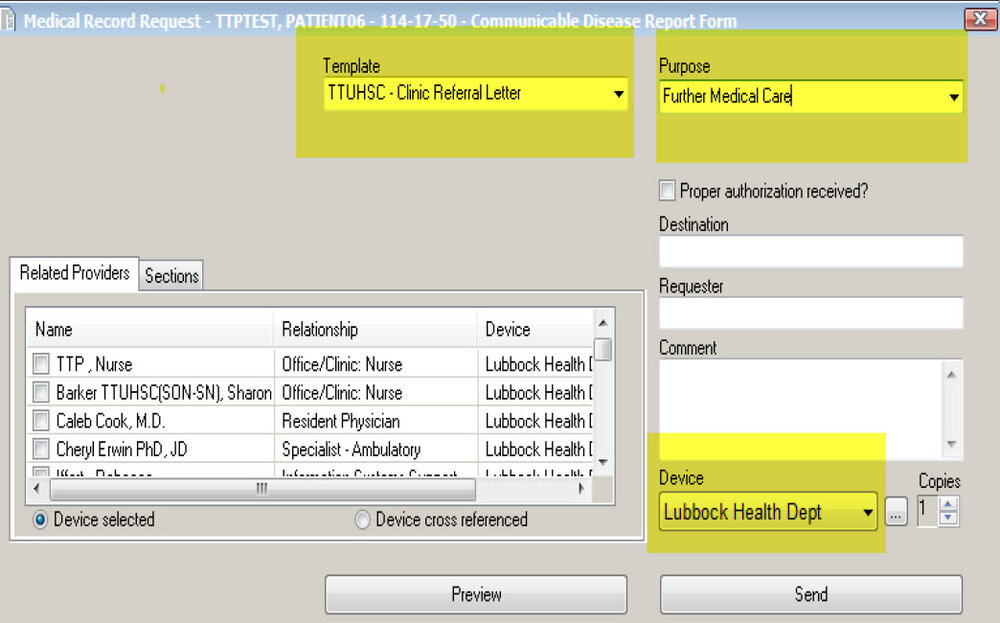
#1) Template: This is automatically set to TTUHSC – CLINIC REFERRAL LETTER.
#2) Purpose: Select FURTHER MEDICAL CARE. This choice will now save as your default.
#3) Device: Type in LUBBOCK HEALTH DEPARTMENT, select this option.
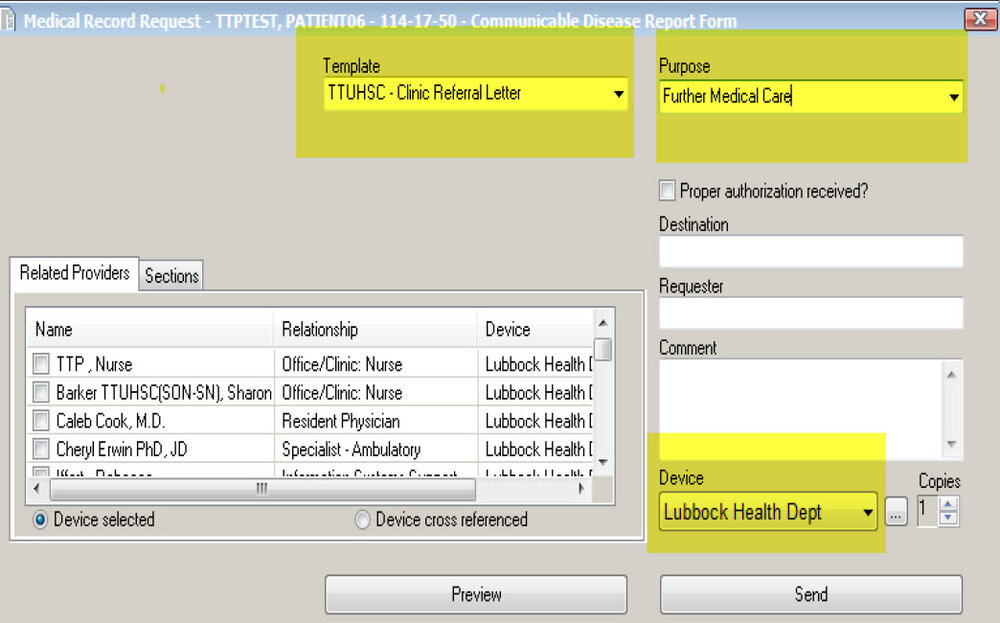
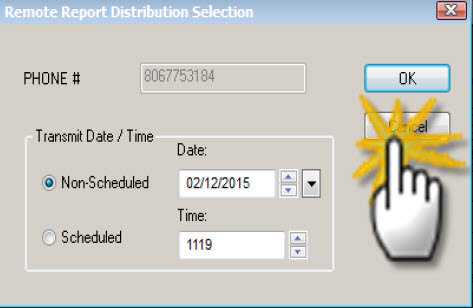
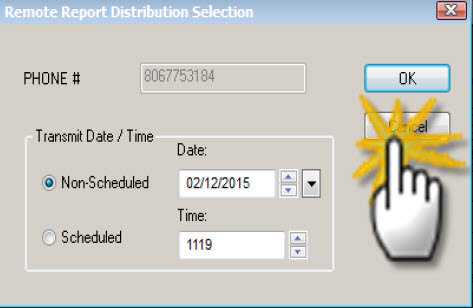
The Remote Report Distribution Selection window will open……NO NOT CHANGE ANY INFORMATION. CLICK OK.
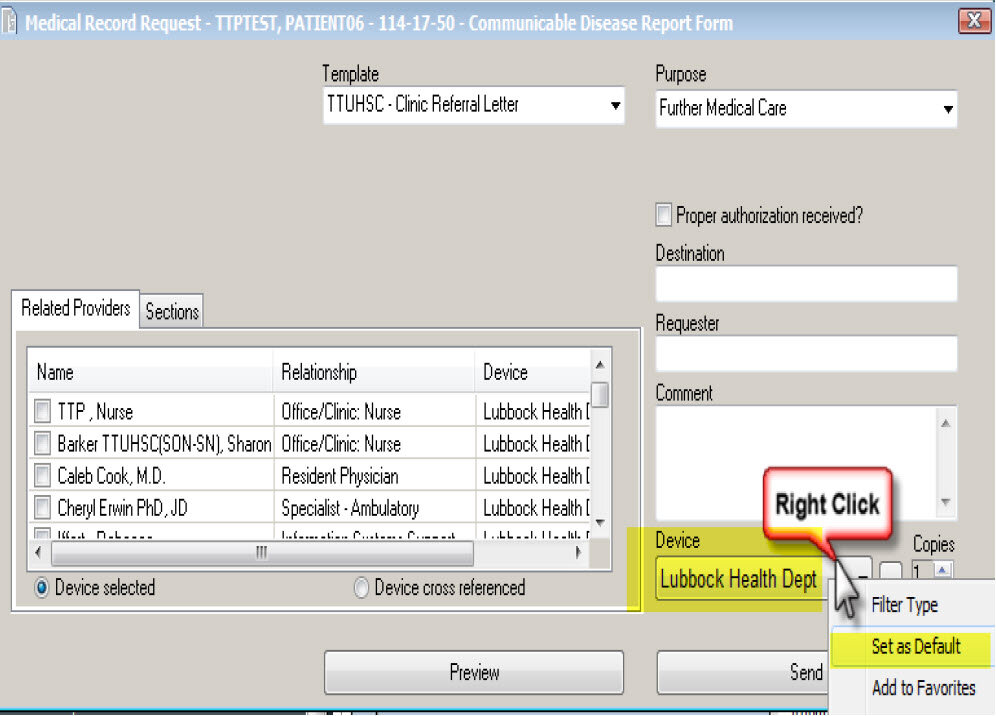
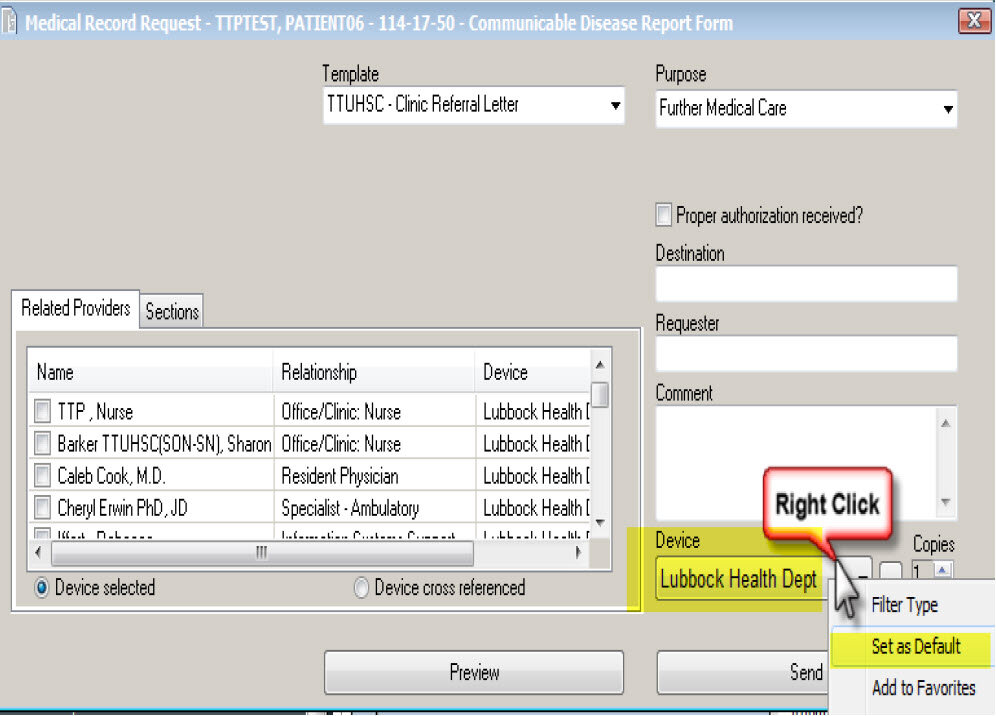
4) The Medical Record Request window will reopen….RIGHT CLICK ON THE LUBBOCK HEALTH DEPARTMENT UNDER THE DEVICE OPTION, AND SET LUBBOCK HEALTH DEPARTMENT AS YOUR DEFAULT (this is a one-time default set)
5) Click SEND.
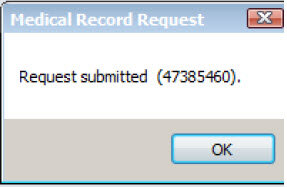
6) Request Submitted window will open. Click OK. Process is completed.