NCPDP SCRIPT ePrescribing Upgrade – 12/10/2019
WHY? CMS has adopted an update to the Medicare Part D electronic prescribing standards from NCPDP 10.6 to NCPDP 2017071 (NCPDP = National Council of Prescription Drug Programs). This requirement has a compliance date of 1/1/2020 and is impactful to any organization that conducts electronic transacting in any of the NCPDP standards in scope of the Part D requirement. UMC will update our ePrescribing standards to the new script on 12/10/2019.
What does this mean for you? On 12/10, you will be asked to log out and back into PowerChart. When you log back in, the upgrade will be complete and you will see the enhancements listed below.
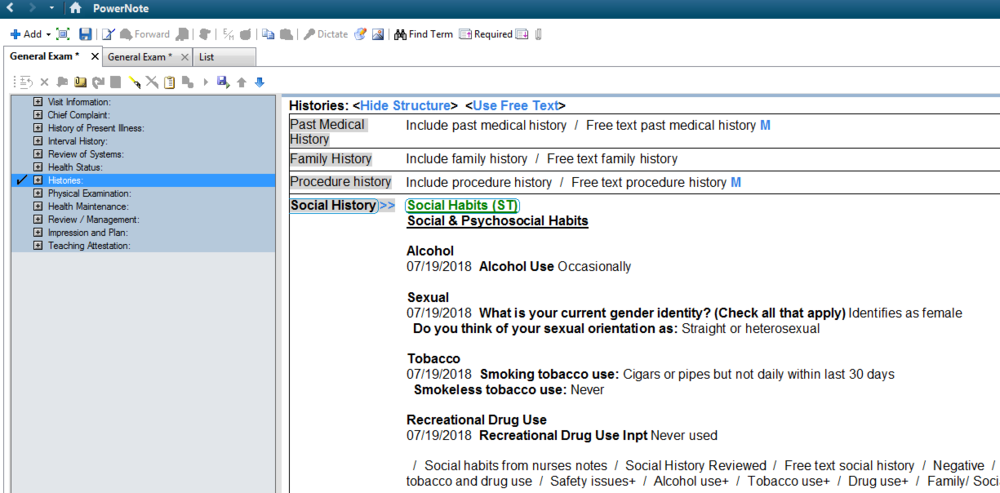
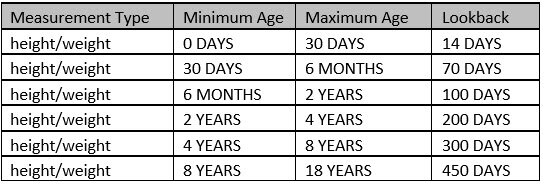
- Transmitting Patient Height and Weight - PowerChart can now support sending a patient’s height and weight on prescriptions. Both pieces of information are always sent when they are available and valid for all patients. The NCPDP SCRIPT standard requires that this information be provided on prescriptions for patients under the age of 18 and the system prevents you from routing a prescription electronically if that information is not available and valid. If the information is not documented or is no longer valid, the system displays a notice on the order scratch pad and in the routing dialogue box. In this case, the height and weight will need to be entered prior to entering the prescription.

- Pediatric physicians across the organization approved the following lookback time periods based on the patient age. For example, a documented weight for an 8-month-old child would only be clinically valid for 100 days. If a provider is trying to send a prescription and the patient has not been seen in the last 100 days, the system will give the error shown above and a weight will have to be entered before the script can be sent.
- Measured height/weight and Estimated height/weight documentation are both acceptable.
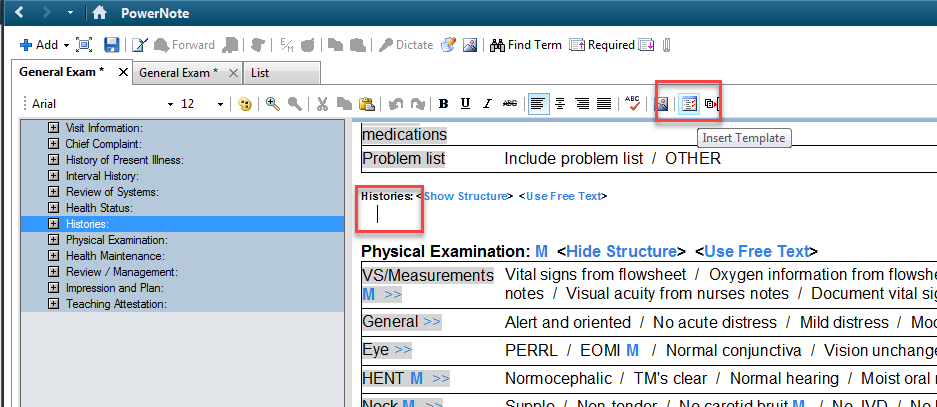
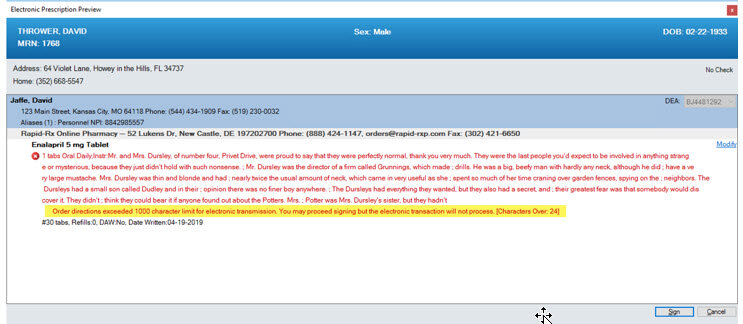
- 1000 Character SIG Support - You can enter a SIG with special instructions up to 1000 characters. If the combination of SIG elements combined with special instructions exceeds 1000 characters, then you cannot route the prescription on the review screen (shown below). If the pharmacy selected in the ordering conversation has not been upgraded, then the system prevents you from exceeding 140 characters on the prescription review screen to ensure the pharmacy can accept your order.
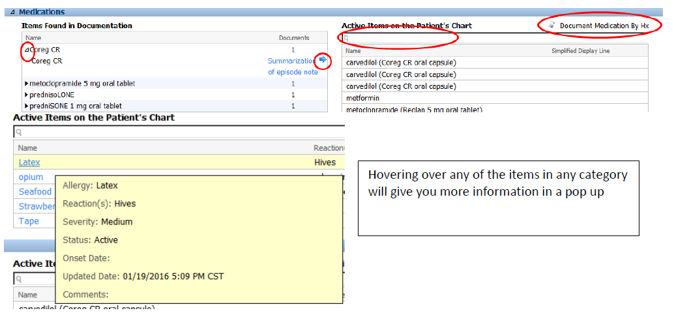
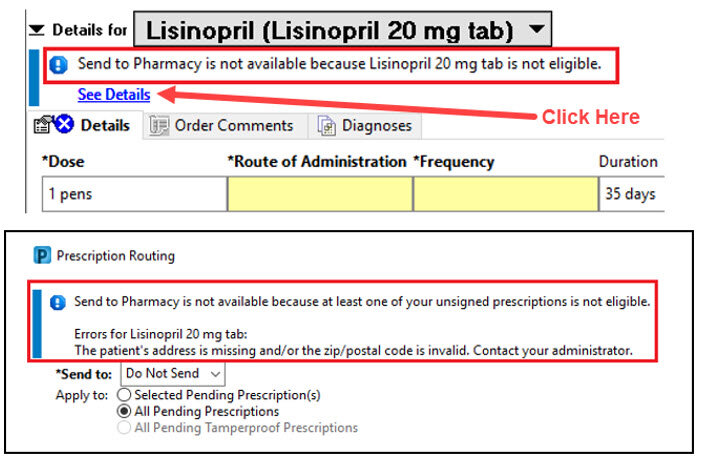
- Enhanced Routing Error Messaging - If an error is present, the system displays an alert in the scratch pad banner and you can click See Details or open the Routing dialogue box to view the specific information. If the error is due to a missing or invalid height and or weight, the system displays that specific error in the scratch pad banner. The error messages encompass all the various reasons why you cannot route orders electronically, whether they be user, patient, facility, or medication specific.
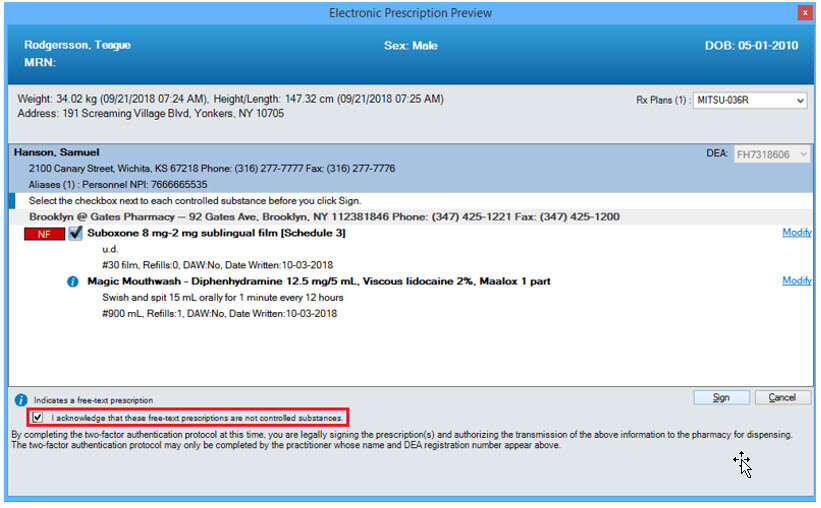
- Prescription Review Screen Updates - A new checkbox has been included at the bottom of the review screen if any free-text prescriptions are included in your ordering conversation. Free-text orders do not meet the DEA’s requirements for transmitting controlled substances and should never include a controlled substance. This box must be selected to indicate that none of your free-text orders contain controlled substances in order to sign the orderable items. If one of the free-text orders does contain a controlled substance then you can select cancel or modify and remove the order from your scratch pad to be ordered correctly with an NDC.