Click the link for a handout tutorial on Advanced Beneficiary Noticies with Medicare patients and Medical Necessity Checking.
What: Patient Status Order (PSO), Medicare Medical Necessity, and Order to Scheduling go-live
When: Go-live will coincide with Cerner Registration & Scheduling go-live, August 4th
Who: All clinicians and end-users who order and/or schedule any radiology orders, PT/OT, Rehab orders (e.g., MRI, CT, US, CV, Mammograms, NM, etc.)
*Does NOT apply to Perinatal Center or GYN ultrasounds or plain DX films
FOR MEDICARE PATIENTS ONLY:
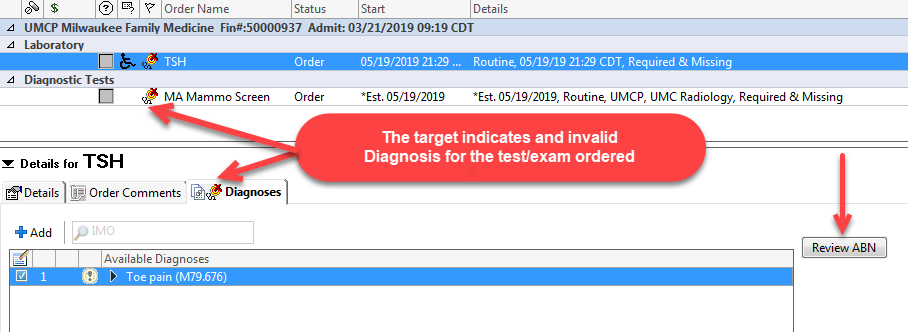
If an inappropriate diagnosis is placed with a testing order, you will have to either:
- Select the proper diagnosis (icon goes away), or
- Fill out the advanced beneficiary notice (ABN) and explain to the patient the cost of the test that will not be covered by Medicare, as the incorrect diagnosis code has been applied
- Diagnosis codes determined by CMS
- Will always qualify for mammogram exams due to frequency rules
- If not addressed, and is a schedulable test, this will be prompt those scheduling the test that an ABN is required
Medical Necessity ABN Checking – In Summary
-
- Qualifies ONLY for Medicare Patients
- CMS defines imaging and lab tests that must have a valid diagnosis
- When a test is ordered without an applicable diagnosis
- A target will appear with a “Review ABN” button
HOW to RESOLVE
-
- Add an applicable diagnosis for each specific order
- OR perform the “Review ABN” process, have form signed and scanned
